Thrombosis
Published: 18 Jun 2025
ICD9: 444.09 ICD10: I74.9 ICD11: BC46
Thrombosis is the formation of a blood clot (thrombus) inside a blood vessel, obstructing the flow of blood through the circulatory system.
Essentially, it's a blood clot that forms where it shouldn't.
Here's a breakdown of key aspects:
![]() What is a Thrombus (Blood Clot)? A thrombus is a solid mass formed from components of blood, including platelets, fibrin, and red blood cells. It's the body's natural response to injury to stop bleeding. However, when a clot forms inappropriately within a blood vessel, it becomes a thrombus.
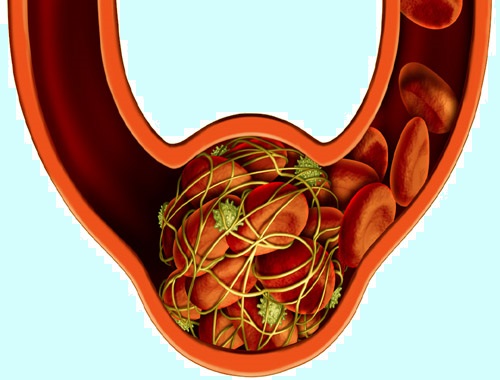
What is a Thrombus (Blood Clot)? A thrombus is a solid mass formed from components of blood, including platelets, fibrin, and red blood cells. It's the body's natural response to injury to stop bleeding. However, when a clot forms inappropriately within a blood vessel, it becomes a thrombus.
![]() Where Can Thrombosis Occur? Thrombosis can happen in both arteries and veins:
Where Can Thrombosis Occur? Thrombosis can happen in both arteries and veins:![]()

![]() Arterial Thrombosis: Occurs in arteries (vessels that carry oxygen-rich blood away from the heart). It often leads to serious consequences because it can suddenly cut off the oxygen supply to vital organs. Examples include:
Arterial Thrombosis: Occurs in arteries (vessels that carry oxygen-rich blood away from the heart). It often leads to serious consequences because it can suddenly cut off the oxygen supply to vital organs. Examples include:![]()

![]() Stroke: A thrombus in an artery in the brain.
Stroke: A thrombus in an artery in the brain.![]()

![]() Heart Attack (Myocardial Infarction): A thrombus in a coronary artery.
Heart Attack (Myocardial Infarction): A thrombus in a coronary artery.![]()

![]() Peripheral Artery Disease (PAD): A thrombus in an artery in the legs or arms.
Peripheral Artery Disease (PAD): A thrombus in an artery in the legs or arms.![]()

![]() Venous Thrombosis: Occurs in veins (vessels that carry blood back to the heart). It's often associated with slower blood flow. The most common types are:
Venous Thrombosis: Occurs in veins (vessels that carry blood back to the heart). It's often associated with slower blood flow. The most common types are:![]()

![]() Deep Vein Thrombosis (DVT): A thrombus that forms in a deep vein, usually in the legs.
Deep Vein Thrombosis (DVT): A thrombus that forms in a deep vein, usually in the legs.![]()

![]() Pulmonary Embolism (PE): A DVT that breaks loose and travels to the lungs, blocking blood flow.
Pulmonary Embolism (PE): A DVT that breaks loose and travels to the lungs, blocking blood flow.
![]() Causes and Risk Factors: Many factors can increase the risk of thrombosis, including:
Causes and Risk Factors: Many factors can increase the risk of thrombosis, including:![]()

![]() Damage to the Blood Vessel Wall: Injury, surgery, inflammation, or atherosclerosis (plaque buildup in arteries) can damage the vessel lining and trigger clot formation.
Damage to the Blood Vessel Wall: Injury, surgery, inflammation, or atherosclerosis (plaque buildup in arteries) can damage the vessel lining and trigger clot formation.![]()

![]() Slow Blood Flow (Stasis): Prolonged inactivity (e.g., sitting for long periods, bed rest after surgery, long flights), varicose veins, or conditions that compress veins can slow blood flow.
Slow Blood Flow (Stasis): Prolonged inactivity (e.g., sitting for long periods, bed rest after surgery, long flights), varicose veins, or conditions that compress veins can slow blood flow.![]()

![]() Hypercoagulability (Increased Tendency to Clot): Certain inherited conditions, medications (e.g., birth control pills, hormone replacement therapy), pregnancy, cancer, and autoimmune diseases can make the blood more likely to clot.
Hypercoagulability (Increased Tendency to Clot): Certain inherited conditions, medications (e.g., birth control pills, hormone replacement therapy), pregnancy, cancer, and autoimmune diseases can make the blood more likely to clot.![]()

![]() Other Risk Factors: Age, obesity, smoking, high cholesterol, and high blood pressure also increase the risk.
Other Risk Factors: Age, obesity, smoking, high cholesterol, and high blood pressure also increase the risk.
![]() Symptoms: Symptoms vary depending on the location of the thrombosis:
Symptoms: Symptoms vary depending on the location of the thrombosis:![]()

![]() Arterial Thrombosis: Sudden, severe pain; numbness; paralysis; coolness; paleness in the affected limb or area. Symptoms often develop quickly.
Arterial Thrombosis: Sudden, severe pain; numbness; paralysis; coolness; paleness in the affected limb or area. Symptoms often develop quickly.![]()

![]() DVT: Pain, swelling, redness, warmth, and tenderness in the leg.
DVT: Pain, swelling, redness, warmth, and tenderness in the leg.![]()

![]() PE: Sudden shortness of breath, chest pain, cough (possibly with blood), rapid heart rate, lightheadedness, and sometimes sudden death.
PE: Sudden shortness of breath, chest pain, cough (possibly with blood), rapid heart rate, lightheadedness, and sometimes sudden death.
![]() Diagnosis: Doctors use various tests to diagnose thrombosis, including:
Diagnosis: Doctors use various tests to diagnose thrombosis, including:![]()

![]() Physical Examination and Medical History: To assess symptoms and risk factors.
Physical Examination and Medical History: To assess symptoms and risk factors.![]()

![]() Blood Tests: D-dimer test (to detect the presence of blood clots), clotting factor tests.
Blood Tests: D-dimer test (to detect the presence of blood clots), clotting factor tests.![]()

![]() Imaging Tests: Ultrasound (for DVT), CT scan or MRI (for PE, arterial clots). Angiography (X-ray of blood vessels after injecting contrast dye).
Imaging Tests: Ultrasound (for DVT), CT scan or MRI (for PE, arterial clots). Angiography (X-ray of blood vessels after injecting contrast dye).
![]() Treatment: The goal of treatment is to prevent the clot from growing, prevent new clots from forming, and, in some cases, dissolve the existing clot. Treatments include:
Treatment: The goal of treatment is to prevent the clot from growing, prevent new clots from forming, and, in some cases, dissolve the existing clot. Treatments include:![]()

![]() Anticoagulants (Blood Thinners): Medications like warfarin, heparin, enoxaparin, and newer oral anticoagulants (DOACs) that prevent clots from forming and growing.
Anticoagulants (Blood Thinners): Medications like warfarin, heparin, enoxaparin, and newer oral anticoagulants (DOACs) that prevent clots from forming and growing.![]()

![]() Thrombolytic Therapy (Clot-Busting Drugs): Medications like tPA (tissue plasminogen activator) that dissolve existing clots. Used in emergency situations like stroke or severe PE.
Thrombolytic Therapy (Clot-Busting Drugs): Medications like tPA (tissue plasminogen activator) that dissolve existing clots. Used in emergency situations like stroke or severe PE.![]()

![]() Compression Stockings: For DVT, to reduce swelling and pain.
Compression Stockings: For DVT, to reduce swelling and pain.![]()

![]() Catheter-Directed Thrombolysis: A catheter is inserted into the blood vessel to deliver thrombolytic drugs directly to the clot.
Catheter-Directed Thrombolysis: A catheter is inserted into the blood vessel to deliver thrombolytic drugs directly to the clot.![]()

![]() Thrombectomy: Surgical removal of the clot.
Thrombectomy: Surgical removal of the clot.![]()

![]() IVC Filter: A filter placed in the inferior vena cava (a large vein in the abdomen) to catch clots that break loose from the legs and prevent them from traveling to the lungs.
IVC Filter: A filter placed in the inferior vena cava (a large vein in the abdomen) to catch clots that break loose from the legs and prevent them from traveling to the lungs.
![]() Prevention: Preventing thrombosis involves managing risk factors:
Prevention: Preventing thrombosis involves managing risk factors:![]()

![]() Lifestyle Modifications: Regular exercise, maintaining a healthy weight, quitting smoking, and controlling blood pressure and cholesterol levels.
Lifestyle Modifications: Regular exercise, maintaining a healthy weight, quitting smoking, and controlling blood pressure and cholesterol levels.![]()

![]() Hydration: Staying adequately hydrated.
Hydration: Staying adequately hydrated.![]()

![]() Movement: Avoiding prolonged sitting or standing. Taking breaks to walk around during long trips.
Movement: Avoiding prolonged sitting or standing. Taking breaks to walk around during long trips.![]()

![]() Anticoagulant Medications: For people at high risk (e.g., after surgery, with certain medical conditions).
Anticoagulant Medications: For people at high risk (e.g., after surgery, with certain medical conditions).![]()

![]() Compression Stockings: For those at risk of DVT.
Compression Stockings: For those at risk of DVT.
In summary, thrombosis is a serious condition that can lead to life-threatening complications. Prompt diagnosis and treatment are crucial. If you suspect you have symptoms of thrombosis, seek medical attention immediately.