Thymoma
Published: 18 Jun 2025
ICD9: 164.0 ICD10: C37 ICD11: 2C27.Y
A thymoma is a rare tumor that originates in the thymus gland.
Here's a breakdown of what that means:
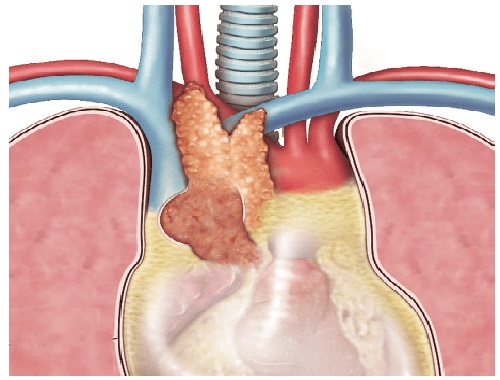
![]() Thymus Gland: The thymus is a small gland located in the upper chest, behind the breastbone and in front of the heart. It is part of the immune system and is most active during childhood. It plays a crucial role in the development and maturation of T lymphocytes (T cells), which are a type of white blood cell that helps the body fight off infections and diseases. After puberty, the thymus starts to shrink and is replaced by fat tissue.
Thymus Gland: The thymus is a small gland located in the upper chest, behind the breastbone and in front of the heart. It is part of the immune system and is most active during childhood. It plays a crucial role in the development and maturation of T lymphocytes (T cells), which are a type of white blood cell that helps the body fight off infections and diseases. After puberty, the thymus starts to shrink and is replaced by fat tissue.
![]() Tumor: A tumor is an abnormal mass of tissue. Tumors can be benign (non-cancerous) or malignant (cancerous).
Tumor: A tumor is an abnormal mass of tissue. Tumors can be benign (non-cancerous) or malignant (cancerous).
![]() Thymoma Defined: Therefore, a thymoma is a tumor arising from the epithelial cells of the thymus. These tumors are rare and can range from slow-growing and encapsulated (contained within a capsule) to more aggressive and invasive.
Thymoma Defined: Therefore, a thymoma is a tumor arising from the epithelial cells of the thymus. These tumors are rare and can range from slow-growing and encapsulated (contained within a capsule) to more aggressive and invasive.
Key characteristics and points about thymomas:
![]() Rarity: Thymomas are relatively rare, accounting for less than 1% of all cancers.
Rarity: Thymomas are relatively rare, accounting for less than 1% of all cancers.
![]() Age of Diagnosis: They are most commonly diagnosed in adults between the ages of 40 and 60.
Age of Diagnosis: They are most commonly diagnosed in adults between the ages of 40 and 60.
![]() Association with Autoimmune Diseases: A significant percentage of people with thymomas also have autoimmune diseases. The most common of these is myasthenia gravis (an autoimmune neuromuscular disorder that causes muscle weakness). Other associated autoimmune diseases include:
Association with Autoimmune Diseases: A significant percentage of people with thymomas also have autoimmune diseases. The most common of these is myasthenia gravis (an autoimmune neuromuscular disorder that causes muscle weakness). Other associated autoimmune diseases include:![]()

![]() Pure red cell aplasia (a blood disorder)
Pure red cell aplasia (a blood disorder)![]()

![]() Hypogammaglobulinemia (a weakened immune system)
Hypogammaglobulinemia (a weakened immune system)![]()

![]() Lupus
Lupus![]()

![]() Rheumatoid arthritis
Rheumatoid arthritis![]()

![]() Sjogren's syndrome
Sjogren's syndrome
![]() Symptoms: Many thymomas are asymptomatic (cause no symptoms) and are discovered incidentally during chest imaging for other reasons. However, symptoms can occur due to the tumor pressing on nearby structures, or due to associated autoimmune diseases. Possible symptoms include:
Symptoms: Many thymomas are asymptomatic (cause no symptoms) and are discovered incidentally during chest imaging for other reasons. However, symptoms can occur due to the tumor pressing on nearby structures, or due to associated autoimmune diseases. Possible symptoms include:![]()

![]() Cough
Cough![]()

![]() Chest pain
Chest pain![]()

![]() Shortness of breath
Shortness of breath![]()

![]() Swallowing difficulties
Swallowing difficulties![]()

![]() Muscle weakness (especially if associated with myasthenia gravis)
Muscle weakness (especially if associated with myasthenia gravis)![]()

![]() Drooping eyelids
Drooping eyelids![]()

![]() Double vision
Double vision
![]() Diagnosis: Diagnosis typically involves:
Diagnosis: Diagnosis typically involves:![]()

![]() Imaging scans (chest X-ray, CT scan, MRI)
Imaging scans (chest X-ray, CT scan, MRI)![]()

![]() Biopsy (removal of a tissue sample for examination under a microscope)
Biopsy (removal of a tissue sample for examination under a microscope)
![]() Treatment: Treatment options depend on the stage, size, and characteristics of the thymoma, as well as the patient's overall health. Common treatments include:
Treatment: Treatment options depend on the stage, size, and characteristics of the thymoma, as well as the patient's overall health. Common treatments include:![]()

![]() Surgery (the primary treatment, especially for early-stage tumors)
Surgery (the primary treatment, especially for early-stage tumors)![]()

![]() Radiation therapy
Radiation therapy![]()

![]() Chemotherapy (usually used for more advanced or aggressive tumors)
Chemotherapy (usually used for more advanced or aggressive tumors)![]()

![]() Immunosuppressant drugs (to manage associated autoimmune diseases)
Immunosuppressant drugs (to manage associated autoimmune diseases)
![]() Prognosis: The prognosis for thymomas varies depending on the stage of the disease and whether it has spread. Early-stage thymomas that are completely removed with surgery have a very good prognosis. More advanced thymomas may require a combination of treatments and have a less favorable outlook.
Prognosis: The prognosis for thymomas varies depending on the stage of the disease and whether it has spread. Early-stage thymomas that are completely removed with surgery have a very good prognosis. More advanced thymomas may require a combination of treatments and have a less favorable outlook.
Important Considerations:
![]() If you are experiencing any symptoms that concern you, especially those related to the chest or unexplained muscle weakness, it is crucial to consult with a doctor for proper evaluation and diagnosis.
If you are experiencing any symptoms that concern you, especially those related to the chest or unexplained muscle weakness, it is crucial to consult with a doctor for proper evaluation and diagnosis.
![]() Information provided here is for educational purposes only and should not be considered as medical advice. Always seek guidance from qualified healthcare professionals for any health concerns.
Information provided here is for educational purposes only and should not be considered as medical advice. Always seek guidance from qualified healthcare professionals for any health concerns.