Type 1 Diabetes
Published: 18 Jun 2025
ICD9: 250.01 ICD10: E10.9 ICD11: 5A10
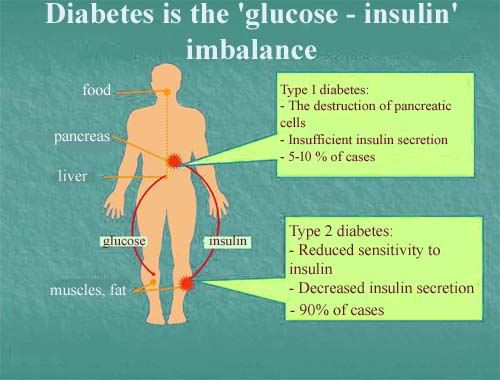
Type 1 diabetes is a chronic autoimmune condition where the body's immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas.
Insulin is a hormone that allows glucose (sugar) from the food we eat to enter cells and be used for energy. Without insulin, glucose builds up in the bloodstream, leading to high blood sugar levels.
Here's a breakdown of the key aspects:
![]() Autoimmune: The body's immune system, which normally fights off infections, attacks its own cells (the beta cells in the pancreas). The reason for this autoimmune attack is not fully understood, but it is thought to involve a combination of genetic predisposition and environmental factors.
Autoimmune: The body's immune system, which normally fights off infections, attacks its own cells (the beta cells in the pancreas). The reason for this autoimmune attack is not fully understood, but it is thought to involve a combination of genetic predisposition and environmental factors.
![]() Insulin Deficiency: Because the beta cells are destroyed, the body cannot produce enough or any insulin. This is the hallmark of type 1 diabetes.
Insulin Deficiency: Because the beta cells are destroyed, the body cannot produce enough or any insulin. This is the hallmark of type 1 diabetes.
![]() High Blood Sugar (Hyperglycemia): Without insulin to help glucose enter cells, it accumulates in the bloodstream. Chronically high blood sugar can lead to a range of serious health problems affecting the heart, kidneys, eyes, nerves, and blood vessels.
High Blood Sugar (Hyperglycemia): Without insulin to help glucose enter cells, it accumulates in the bloodstream. Chronically high blood sugar can lead to a range of serious health problems affecting the heart, kidneys, eyes, nerves, and blood vessels.
![]() Lifelong Condition: Type 1 diabetes is a lifelong condition that requires regular monitoring of blood sugar levels and insulin therapy to manage blood sugar levels and prevent complications.
Lifelong Condition: Type 1 diabetes is a lifelong condition that requires regular monitoring of blood sugar levels and insulin therapy to manage blood sugar levels and prevent complications.
Key characteristics:
![]() Usually diagnosed in childhood or adolescence, but can occur at any age.
Usually diagnosed in childhood or adolescence, but can occur at any age.
![]() Not related to lifestyle factors like diet or exercise. It's an autoimmune disease.
Not related to lifestyle factors like diet or exercise. It's an autoimmune disease.
![]() Requires insulin therapy for survival. People with type 1 diabetes need to take insulin via injections, insulin pens, or insulin pumps multiple times a day.
Requires insulin therapy for survival. People with type 1 diabetes need to take insulin via injections, insulin pens, or insulin pumps multiple times a day.
![]() Symptoms can develop quickly, often over a period of weeks or months.
Symptoms can develop quickly, often over a period of weeks or months.
Common Symptoms:
![]() Frequent urination: Especially at night.
Frequent urination: Especially at night.
![]() Excessive thirst
Excessive thirst
![]() Unexplained weight loss: Even though you're eating more.
Unexplained weight loss: Even though you're eating more.
![]() Increased hunger
Increased hunger
![]() Fatigue and weakness
Fatigue and weakness
![]() Blurred vision
Blurred vision
![]() Slow-healing sores
Slow-healing sores
![]() Frequent infections
Frequent infections
![]() Dry, itchy skin
Dry, itchy skin
Management:
Management of type 1 diabetes involves a comprehensive approach that includes:
![]() Insulin therapy: To replace the insulin the body cannot produce.
Insulin therapy: To replace the insulin the body cannot produce.
![]() Blood sugar monitoring: Regularly checking blood sugar levels using a glucose meter or continuous glucose monitor (CGM).
Blood sugar monitoring: Regularly checking blood sugar levels using a glucose meter or continuous glucose monitor (CGM).
![]() Carbohydrate counting: Learning how to estimate the amount of carbohydrates in food and adjusting insulin doses accordingly.
Carbohydrate counting: Learning how to estimate the amount of carbohydrates in food and adjusting insulin doses accordingly.
![]() Healthy eating: Following a balanced diet that is low in processed foods, sugary drinks, and unhealthy fats.
Healthy eating: Following a balanced diet that is low in processed foods, sugary drinks, and unhealthy fats.
![]() Regular exercise: Helps improve insulin sensitivity and control blood sugar levels.
Regular exercise: Helps improve insulin sensitivity and control blood sugar levels.
![]() Regular checkups: Seeing a healthcare team regularly for monitoring and to address any potential complications.
Regular checkups: Seeing a healthcare team regularly for monitoring and to address any potential complications.
It is important to note that this is a simplified explanation. It's crucial to consult with healthcare professionals for accurate diagnosis, treatment, and management of type 1 diabetes.