Type 2 Diabetes
Published: 18 Jun 2025
ICD9: 250.00 ICD10: E11.9 ICD11: 5A11
Type 2 diabetes is a chronic metabolic disorder characterized by high blood sugar (glucose) levels due to the body's ineffective use of insulin.
Insulin is a hormone produced by the pancreas that helps glucose from food enter cells to be used for energy. In type 2 diabetes, the body either doesn't produce enough insulin or the cells become resistant to insulin (insulin resistance).
Here's a breakdown of key aspects:
![]() Insulin Resistance: This is a primary feature. The body's cells (muscle, fat, and liver cells) don't respond properly to insulin. This means that even when insulin is present, glucose struggles to enter the cells.
Insulin Resistance: This is a primary feature. The body's cells (muscle, fat, and liver cells) don't respond properly to insulin. This means that even when insulin is present, glucose struggles to enter the cells.
![]() Insulin Deficiency: Over time, the pancreas may not be able to produce enough insulin to overcome the insulin resistance and keep blood sugar levels in a normal range.
Insulin Deficiency: Over time, the pancreas may not be able to produce enough insulin to overcome the insulin resistance and keep blood sugar levels in a normal range.
![]() High Blood Sugar (Hyperglycemia): Because glucose can't easily enter cells, it builds up in the bloodstream, leading to hyperglycemia.
High Blood Sugar (Hyperglycemia): Because glucose can't easily enter cells, it builds up in the bloodstream, leading to hyperglycemia.
Causes and Risk Factors:
Type 2 diabetes is often a result of a combination of genetic predisposition and lifestyle factors. Key risk factors include:
![]() Weight: Being overweight or obese, especially having excess abdominal fat.
Weight: Being overweight or obese, especially having excess abdominal fat.
![]() Inactivity: Lack of physical activity.
Inactivity: Lack of physical activity.
![]() Family History: Having a parent or sibling with type 2 diabetes.
Family History: Having a parent or sibling with type 2 diabetes.
![]() Age: Risk increases with age, especially after 45.
Age: Risk increases with age, especially after 45.
![]() Ethnicity: Some ethnic groups (African Americans, Hispanics/Latinos, Native Americans, Asian Americans, and Pacific Islanders) have a higher risk.
Ethnicity: Some ethnic groups (African Americans, Hispanics/Latinos, Native Americans, Asian Americans, and Pacific Islanders) have a higher risk.
![]() Prediabetes: Having blood sugar levels higher than normal but not high enough to be diagnosed with diabetes.
Prediabetes: Having blood sugar levels higher than normal but not high enough to be diagnosed with diabetes.
![]() Gestational Diabetes: Having diabetes during pregnancy.
Gestational Diabetes: Having diabetes during pregnancy.
![]() Polycystic Ovary Syndrome (PCOS): A hormonal disorder common in women.
Polycystic Ovary Syndrome (PCOS): A hormonal disorder common in women.
Symptoms:
Symptoms of type 2 diabetes can develop gradually and may not be noticeable at first. Some people may not experience any symptoms at all in the early stages. Common symptoms include:
![]() Increased thirst
Increased thirst
![]() Frequent urination (especially at night)
Frequent urination (especially at night)
![]() Increased hunger
Increased hunger
![]() Unexplained weight loss
Unexplained weight loss
![]() Fatigue
Fatigue
![]() Blurred vision
Blurred vision
![]() Slow-healing sores
Slow-healing sores
![]() Frequent infections
Frequent infections
![]() Areas of darkened skin, usually in the armpits and neck (acanthosis nigricans)
Areas of darkened skin, usually in the armpits and neck (acanthosis nigricans)
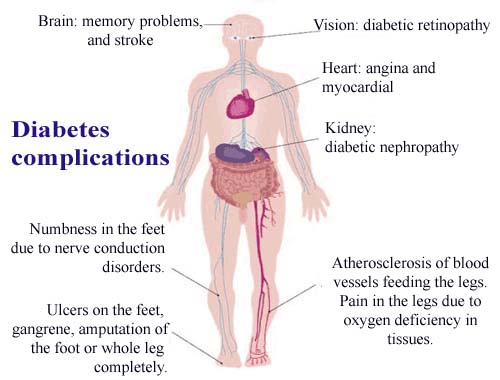
Complications:
If left untreated or poorly managed, type 2 diabetes can lead to serious long-term complications, including:
![]() Cardiovascular disease: Heart attack, stroke, high blood pressure, and high cholesterol.
Cardiovascular disease: Heart attack, stroke, high blood pressure, and high cholesterol.
![]() Neuropathy: Nerve damage, causing numbness, tingling, or pain in the hands and feet.
Neuropathy: Nerve damage, causing numbness, tingling, or pain in the hands and feet.
![]() Nephropathy: Kidney damage, which can lead to kidney failure.
Nephropathy: Kidney damage, which can lead to kidney failure.
![]() Retinopathy: Eye damage, which can lead to blindness.
Retinopathy: Eye damage, which can lead to blindness.
![]() Foot problems: Poor circulation and nerve damage can lead to foot ulcers and infections, sometimes requiring amputation.
Foot problems: Poor circulation and nerve damage can lead to foot ulcers and infections, sometimes requiring amputation.
![]() Skin conditions: Increased susceptibility to skin infections.
Skin conditions: Increased susceptibility to skin infections.
![]() Hearing impairment
Hearing impairment
![]() Alzheimer's disease
Alzheimer's disease
Diagnosis:
Diabetes is typically diagnosed through blood tests that measure blood glucose levels. Common tests include:
![]() Fasting Plasma Glucose (FPG) Test: Measures blood glucose after an overnight fast.
Fasting Plasma Glucose (FPG) Test: Measures blood glucose after an overnight fast.
![]() Oral Glucose Tolerance Test (OGTT): Measures blood glucose levels before and after drinking a sugary drink.
Oral Glucose Tolerance Test (OGTT): Measures blood glucose levels before and after drinking a sugary drink.
![]() A1C Test: Reflects average blood glucose levels over the past 2-3 months.
A1C Test: Reflects average blood glucose levels over the past 2-3 months.
Management:
Type 2 diabetes management focuses on controlling blood sugar levels and preventing complications. Treatment typically involves:
![]() Lifestyle Modifications:
Lifestyle Modifications:![]()

![]() Diet: Following a healthy eating plan that emphasizes fruits, vegetables, whole grains, and lean protein. Limiting sugary drinks, processed foods, and saturated and trans fats.
Diet: Following a healthy eating plan that emphasizes fruits, vegetables, whole grains, and lean protein. Limiting sugary drinks, processed foods, and saturated and trans fats.![]()

![]() Exercise: Regular physical activity helps improve insulin sensitivity and lower blood sugar levels.
Exercise: Regular physical activity helps improve insulin sensitivity and lower blood sugar levels.![]()

![]() Weight Management: Losing weight, if overweight or obese, can significantly improve blood sugar control.
Weight Management: Losing weight, if overweight or obese, can significantly improve blood sugar control.
![]() Medications: If lifestyle changes are not enough to control blood sugar, medications may be prescribed. These can include oral medications that help improve insulin sensitivity, stimulate insulin production, or slow the absorption of glucose, as well as injectable medications, including insulin.
Medications: If lifestyle changes are not enough to control blood sugar, medications may be prescribed. These can include oral medications that help improve insulin sensitivity, stimulate insulin production, or slow the absorption of glucose, as well as injectable medications, including insulin.
![]() Regular Monitoring: Monitoring blood glucose levels regularly helps to track the effectiveness of treatment and make adjustments as needed.
Regular Monitoring: Monitoring blood glucose levels regularly helps to track the effectiveness of treatment and make adjustments as needed.
![]() Regular Checkups: Regular medical checkups are important to monitor for complications and ensure that treatment is effective.
Regular Checkups: Regular medical checkups are important to monitor for complications and ensure that treatment is effective.
Prevention:
Type 2 diabetes can often be prevented or delayed through lifestyle changes, such as:
![]() Maintaining a healthy weight
Maintaining a healthy weight
![]() Eating a healthy diet
Eating a healthy diet
![]() Engaging in regular physical activity
Engaging in regular physical activity
![]() Managing stress
Managing stress
![]() Getting enough sleep
Getting enough sleep
In summary, Type 2 diabetes is a complex condition that requires ongoing management. Early diagnosis and treatment can help prevent or delay serious complications and improve quality of life. If you have any concerns about diabetes, it's important to talk to your doctor.