Ulcerative Colitis (Inflammatory Bowel Disease, IBD)
Published: 18 Jun 2025
ICD9: 556.9 ICD10: K51.90 ICD11: DD71
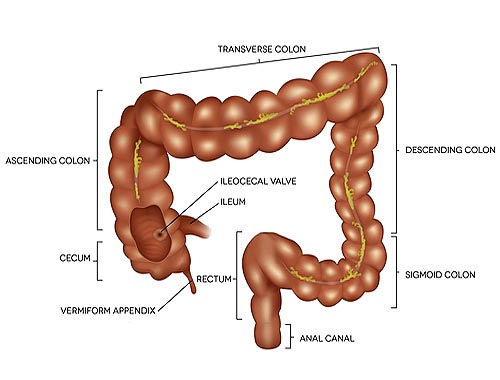
Ulcerative Colitis (UC) is a chronic inflammatory bowel disease (IBD) that causes inflammation and ulcers (sores) in the innermost lining of your large intestine (colon) and rectum.
It's a type of IBD, distinct from Crohn's disease, though they share some overlapping symptoms.
Here's a breakdown of key aspects:
What Happens in Ulcerative Colitis:
![]() Inflammation: The immune system mistakenly attacks the lining of the colon and rectum, causing inflammation.
Inflammation: The immune system mistakenly attacks the lining of the colon and rectum, causing inflammation.
![]() Ulcers: This inflammation leads to the formation of ulcers (sores) on the inner lining.
Ulcers: This inflammation leads to the formation of ulcers (sores) on the inner lining.
![]() Location: UC typically affects the rectum and may extend continuously to involve part or all of the colon. The extent of involvement varies from person to person. It *only* affects the colon and rectum; it does not affect other parts of the digestive tract like Crohn's disease can.
Location: UC typically affects the rectum and may extend continuously to involve part or all of the colon. The extent of involvement varies from person to person. It *only* affects the colon and rectum; it does not affect other parts of the digestive tract like Crohn's disease can.
![]() Continuous Pattern: Unlike Crohn's disease, where inflammation can occur in patches (skip lesions), UC typically presents as a continuous inflammation of the colon and rectum.
Continuous Pattern: Unlike Crohn's disease, where inflammation can occur in patches (skip lesions), UC typically presents as a continuous inflammation of the colon and rectum.
Symptoms:
The severity of symptoms can vary greatly, depending on the extent of inflammation and the individual. Common symptoms include:
![]() Diarrhea: Often bloody and/or containing pus. This is a hallmark symptom.
Diarrhea: Often bloody and/or containing pus. This is a hallmark symptom.
![]() Abdominal pain and cramping: Can range from mild discomfort to severe pain.
Abdominal pain and cramping: Can range from mild discomfort to severe pain.
![]() Rectal pain: May feel like a constant ache or a sharp, stabbing pain.
Rectal pain: May feel like a constant ache or a sharp, stabbing pain.
![]() Rectal bleeding: May be mild or severe.
Rectal bleeding: May be mild or severe.
![]() Urgent need to defecate: A strong and sudden urge to have a bowel movement.
Urgent need to defecate: A strong and sudden urge to have a bowel movement.
![]() Inability to defecate despite urgency: Feeling like you need to go but being unable to.
Inability to defecate despite urgency: Feeling like you need to go but being unable to.
![]() Weight loss: Due to poor absorption of nutrients and decreased appetite.
Weight loss: Due to poor absorption of nutrients and decreased appetite.
![]() Fatigue: A common symptom due to chronic inflammation and anemia.
Fatigue: A common symptom due to chronic inflammation and anemia.
![]() Fever: May occur during flare-ups.
Fever: May occur during flare-ups.
![]() Anemia: Due to chronic blood loss in the stool.
Anemia: Due to chronic blood loss in the stool.
Extraintestinal Manifestations (Symptoms outside the Colon):
UC can sometimes affect other parts of the body, leading to:
![]() Joint pain (arthritis)
Joint pain (arthritis)
![]() Skin problems (rashes, ulcers)
Skin problems (rashes, ulcers)
![]() Eye inflammation (uveitis)
Eye inflammation (uveitis)
![]() Liver problems (rarely)
Liver problems (rarely)
Causes:
The exact cause of UC is unknown, but it's believed to be a combination of factors:
![]() Genetics: People with a family history of IBD are at higher risk.
Genetics: People with a family history of IBD are at higher risk.
![]() Immune System Dysfunction: The immune system attacks the lining of the colon for unknown reasons.
Immune System Dysfunction: The immune system attacks the lining of the colon for unknown reasons.
![]() Environmental Factors: Diet, stress, and infections may play a role in triggering the disease or exacerbating symptoms. However, there's no single known environmental trigger.
Environmental Factors: Diet, stress, and infections may play a role in triggering the disease or exacerbating symptoms. However, there's no single known environmental trigger.
![]() Gut Microbiome: Changes in the balance of bacteria in the gut may contribute to inflammation.
Gut Microbiome: Changes in the balance of bacteria in the gut may contribute to inflammation.
Diagnosis:
Diagnosing UC typically involves a combination of:
![]() Medical History and Physical Exam: The doctor will ask about your symptoms, medical history, and family history.
Medical History and Physical Exam: The doctor will ask about your symptoms, medical history, and family history.
![]() Blood Tests: To check for anemia, inflammation, and infection.
Blood Tests: To check for anemia, inflammation, and infection.
![]() Stool Tests: To rule out infections and look for blood or pus.
Stool Tests: To rule out infections and look for blood or pus.
![]() Colonoscopy: A procedure where a long, flexible tube with a camera is inserted into the rectum and colon to visualize the lining. Biopsies (tissue samples) are taken during the colonoscopy to confirm the diagnosis and assess the severity of inflammation.
Colonoscopy: A procedure where a long, flexible tube with a camera is inserted into the rectum and colon to visualize the lining. Biopsies (tissue samples) are taken during the colonoscopy to confirm the diagnosis and assess the severity of inflammation.
![]() Sigmoidoscopy: Similar to colonoscopy but only examines the rectum and lower part of the colon. Used if colonoscopy is not feasible or only lower colon involvement is suspected.
Sigmoidoscopy: Similar to colonoscopy but only examines the rectum and lower part of the colon. Used if colonoscopy is not feasible or only lower colon involvement is suspected.
![]() Imaging Tests (e.g., CT scan, MRI): May be used to rule out other conditions or assess the extent of the disease.
Imaging Tests (e.g., CT scan, MRI): May be used to rule out other conditions or assess the extent of the disease.
Treatment:
There's no cure for UC, but treatment aims to:
![]() Reduce inflammation:
Reduce inflammation:
![]() Relieve symptoms:
Relieve symptoms:
![]() Prevent flare-ups:
Prevent flare-ups:
![]() Improve quality of life:
Improve quality of life:
Treatment options include:
![]() Medications:
Medications:![]()

![]() Aminosalicylates (5-ASAs): Anti-inflammatory drugs that are often the first-line treatment for mild to moderate UC (e.g., mesalamine, sulfasalazine).
Aminosalicylates (5-ASAs): Anti-inflammatory drugs that are often the first-line treatment for mild to moderate UC (e.g., mesalamine, sulfasalazine).![]()

![]() Corticosteroids: Powerful anti-inflammatory drugs used to quickly reduce inflammation during flare-ups (e.g., prednisone). They are not suitable for long-term use due to side effects.
Corticosteroids: Powerful anti-inflammatory drugs used to quickly reduce inflammation during flare-ups (e.g., prednisone). They are not suitable for long-term use due to side effects.![]()

![]() Immunomodulators: Suppress the immune system to reduce inflammation (e.g., azathioprine, 6-mercaptopurine). They take several weeks or months to work.
Immunomodulators: Suppress the immune system to reduce inflammation (e.g., azathioprine, 6-mercaptopurine). They take several weeks or months to work.![]()

![]() Biologics: Target specific proteins in the immune system that contribute to inflammation (e.g., infliximab, adalimumab, vedolizumab, ustekinumab). These are often used when other medications are not effective.
Biologics: Target specific proteins in the immune system that contribute to inflammation (e.g., infliximab, adalimumab, vedolizumab, ustekinumab). These are often used when other medications are not effective.![]()

![]() Small molecule inhibitors: (e.g. tofacitinib). These medications work inside the cells to block inflammatory pathways.
Small molecule inhibitors: (e.g. tofacitinib). These medications work inside the cells to block inflammatory pathways.
![]() Surgery:
Surgery:![]()

![]() Proctocolectomy with ileal pouch-anal anastomosis (IPAA) (J-pouch surgery): The entire colon and rectum are removed, and a pouch is created from the small intestine and connected to the anus. This allows for normal bowel movements without the need for an ostomy bag. This is often considered the gold standard if medications are ineffective.
Proctocolectomy with ileal pouch-anal anastomosis (IPAA) (J-pouch surgery): The entire colon and rectum are removed, and a pouch is created from the small intestine and connected to the anus. This allows for normal bowel movements without the need for an ostomy bag. This is often considered the gold standard if medications are ineffective.![]()

![]() Proctocolectomy with ileostomy: The entire colon, rectum, and anus are removed. The end of the small intestine (ileum) is brought through an opening in the abdomen (stoma), and stool is collected in an external ostomy bag.
Proctocolectomy with ileostomy: The entire colon, rectum, and anus are removed. The end of the small intestine (ileum) is brought through an opening in the abdomen (stoma), and stool is collected in an external ostomy bag.
![]() Dietary Changes: While diet doesn't cause UC, certain foods can trigger symptoms. Working with a registered dietitian can help identify trigger foods and develop a balanced diet. Common trigger foods include dairy, high-fiber foods, spicy foods, and processed foods. During flare-ups, a low-fiber diet may be recommended.
Dietary Changes: While diet doesn't cause UC, certain foods can trigger symptoms. Working with a registered dietitian can help identify trigger foods and develop a balanced diet. Common trigger foods include dairy, high-fiber foods, spicy foods, and processed foods. During flare-ups, a low-fiber diet may be recommended.
![]() Lifestyle Modifications:
Lifestyle Modifications:![]()

![]() Stress management: Stress can worsen symptoms. Techniques like yoga, meditation, and deep breathing can help.
Stress management: Stress can worsen symptoms. Techniques like yoga, meditation, and deep breathing can help.![]()

![]() Regular exercise: Can improve overall health and reduce stress.
Regular exercise: Can improve overall health and reduce stress.![]()

![]() Smoking cessation: Smoking can worsen UC.
Smoking cessation: Smoking can worsen UC.
Important Considerations:
![]() Flare-ups and Remission: UC is characterized by periods of active symptoms (flare-ups) and periods of remission (when symptoms are minimal or absent).
Flare-ups and Remission: UC is characterized by periods of active symptoms (flare-ups) and periods of remission (when symptoms are minimal or absent).
![]() Increased Risk of Colon Cancer: People with UC have an increased risk of colon cancer, especially if the disease has been present for many years and involves a large portion of the colon. Regular colonoscopies with biopsies are recommended for screening.
Increased Risk of Colon Cancer: People with UC have an increased risk of colon cancer, especially if the disease has been present for many years and involves a large portion of the colon. Regular colonoscopies with biopsies are recommended for screening.
![]() Complications: Possible complications of UC include severe bleeding, toxic megacolon (a life-threatening complication where the colon becomes severely distended), perforation of the colon, and primary sclerosing cholangitis (a liver disease).
Complications: Possible complications of UC include severe bleeding, toxic megacolon (a life-threatening complication where the colon becomes severely distended), perforation of the colon, and primary sclerosing cholangitis (a liver disease).
![]() Importance of Adherence to Treatment: It's crucial to follow your doctor's treatment plan and take medications as prescribed, even when you're feeling well, to maintain remission and prevent complications.
Importance of Adherence to Treatment: It's crucial to follow your doctor's treatment plan and take medications as prescribed, even when you're feeling well, to maintain remission and prevent complications.
In summary, Ulcerative Colitis is a chronic inflammatory bowel disease that affects the colon and rectum, causing inflammation, ulcers, and a range of symptoms. While there's no cure, treatment can effectively manage symptoms, prevent complications, and improve the quality of life for those affected.
Disclaimer: This information is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.