Urethral cancer
Published: 18 Jun 2025
ICD9: 189.3 ICD10: C68.0 ICD11: 2C93
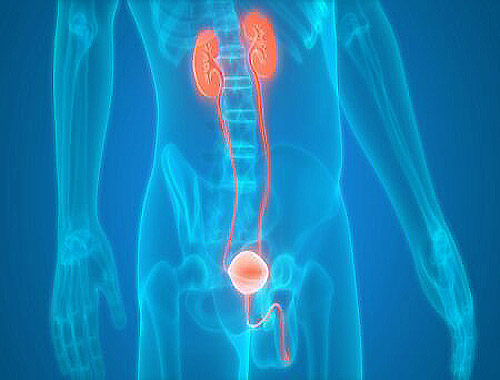
Urethral cancer is a rare type of cancer that forms in the cells of the urethra, the tube that carries urine from the bladder out of the body.
Here's a breakdown of what you should know about it:
Key Aspects:
![]() Rarity: It's a relatively uncommon cancer, accounting for a small percentage of all urologic cancers.
Rarity: It's a relatively uncommon cancer, accounting for a small percentage of all urologic cancers.
![]() Location: It affects the urethra, which is a short tube in women and a longer tube in men (running through the penis).
Location: It affects the urethra, which is a short tube in women and a longer tube in men (running through the penis).
![]() Types: There are different types of urethral cancer, classified by the type of cells involved:
Types: There are different types of urethral cancer, classified by the type of cells involved:![]()

![]() Transitional cell carcinoma (also called urothelial carcinoma): This is the most common type, and it's the same type of cancer that often occurs in the bladder.
Transitional cell carcinoma (also called urothelial carcinoma): This is the most common type, and it's the same type of cancer that often occurs in the bladder.![]()

![]() Squamous cell carcinoma: This type is more common in the urethra that passes through the penis or near the opening of the urethra, especially in areas with a history of chronic irritation or infection.
Squamous cell carcinoma: This type is more common in the urethra that passes through the penis or near the opening of the urethra, especially in areas with a history of chronic irritation or infection.![]()

![]() Adenocarcinoma: This type develops from gland cells in the urethra.
Adenocarcinoma: This type develops from gland cells in the urethra.![]()

![]() Other rare types: Include melanoma and sarcoma.
Other rare types: Include melanoma and sarcoma.
Symptoms:
Urethral cancer symptoms can be subtle and may be mistaken for other conditions. They can include:
![]() Blood in the urine (hematuria): This is one of the most common symptoms.
Blood in the urine (hematuria): This is one of the most common symptoms.
![]() Pain or burning during urination (dysuria)
Pain or burning during urination (dysuria)
![]() Frequent urination
Frequent urination
![]() Difficulty urinating (hesitancy, weak stream)
Difficulty urinating (hesitancy, weak stream)
![]() A lump or mass that can be felt in the perineum (the area between the anus and the genitals)
A lump or mass that can be felt in the perineum (the area between the anus and the genitals)
![]() Discharge from the urethra
Discharge from the urethra
![]() Swollen lymph nodes in the groin area
Swollen lymph nodes in the groin area
![]() In men: Blood in semen.
In men: Blood in semen.
Causes and Risk Factors:
The exact causes of urethral cancer are not fully understood, but some risk factors have been identified:
![]() Age: The risk increases with age.
Age: The risk increases with age.
![]() Gender: Urethral cancer is more common in men than in women.
Gender: Urethral cancer is more common in men than in women.
![]() History of bladder cancer: Having had bladder cancer, especially transitional cell carcinoma, increases the risk of urethral cancer.
History of bladder cancer: Having had bladder cancer, especially transitional cell carcinoma, increases the risk of urethral cancer.
![]() Chronic urethral irritation or inflammation: This can be caused by:
Chronic urethral irritation or inflammation: This can be caused by:![]()

![]() Recurrent urinary tract infections (UTIs)
Recurrent urinary tract infections (UTIs)![]()

![]() Sexually transmitted infections (STIs)
Sexually transmitted infections (STIs)![]()

![]() Urethral strictures (narrowing of the urethra)
Urethral strictures (narrowing of the urethra)![]()

![]() Lichen sclerosus (a skin condition that can affect the genital area)
Lichen sclerosus (a skin condition that can affect the genital area)
![]() Human papillomavirus (HPV) infection: Some types of HPV are linked to urethral cancer, particularly squamous cell carcinoma.
Human papillomavirus (HPV) infection: Some types of HPV are linked to urethral cancer, particularly squamous cell carcinoma.
![]() Smoking: Smoking is a risk factor for many cancers, including urethral cancer.
Smoking: Smoking is a risk factor for many cancers, including urethral cancer.
![]() Radiation therapy to the pelvic area: Past radiation treatment can increase the risk.
Radiation therapy to the pelvic area: Past radiation treatment can increase the risk.
![]() Schistosomiasis: A parasitic infection common in some parts of the world.
Schistosomiasis: A parasitic infection common in some parts of the world.
Diagnosis:
If a doctor suspects urethral cancer, they may perform the following tests:
![]() Physical exam: Includes examining the urethra and surrounding areas.
Physical exam: Includes examining the urethra and surrounding areas.
![]() Urinalysis: To check for blood or other abnormalities in the urine.
Urinalysis: To check for blood or other abnormalities in the urine.
![]() Urine cytology: Examining urine samples under a microscope to look for cancer cells.
Urine cytology: Examining urine samples under a microscope to look for cancer cells.
![]() Cystoscopy and urethroscopy: A thin, flexible tube with a camera (cystoscope or urethroscope) is inserted into the urethra to visualize the lining of the urethra and bladder.
Cystoscopy and urethroscopy: A thin, flexible tube with a camera (cystoscope or urethroscope) is inserted into the urethra to visualize the lining of the urethra and bladder.
![]() Biopsy: A small tissue sample is taken from any suspicious areas during cystoscopy/urethroscopy and examined under a microscope to confirm the diagnosis and determine the type of cancer.
Biopsy: A small tissue sample is taken from any suspicious areas during cystoscopy/urethroscopy and examined under a microscope to confirm the diagnosis and determine the type of cancer.
![]() Imaging tests:
Imaging tests:![]()

![]() CT scan (computed tomography): To assess the extent of the cancer and check for spread to other areas.
CT scan (computed tomography): To assess the extent of the cancer and check for spread to other areas.![]()

![]() MRI (magnetic resonance imaging): Provides detailed images of the urethra and surrounding tissues.
MRI (magnetic resonance imaging): Provides detailed images of the urethra and surrounding tissues.![]()

![]() PET scan (positron emission tomography): Can help detect cancer that has spread to other parts of the body.
PET scan (positron emission tomography): Can help detect cancer that has spread to other parts of the body.
Staging:
Once urethral cancer is diagnosed, it's staged to determine how far it has spread. Staging helps doctors plan the best treatment approach. The stages range from Stage 0 (very early) to Stage IV (advanced, with spread to distant organs).
Treatment:
Treatment for urethral cancer depends on the stage, location, and type of cancer, as well as the patient's overall health. Options may include:
![]() Surgery:
Surgery:![]()

![]() Local excision: Removal of the tumor and a small amount of surrounding tissue. This may be suitable for early-stage cancers.
Local excision: Removal of the tumor and a small amount of surrounding tissue. This may be suitable for early-stage cancers.![]()

![]() Partial or total urethrectomy: Removal of part or all of the urethra. In men, this may involve removing the penis (penectomy).
Partial or total urethrectomy: Removal of part or all of the urethra. In men, this may involve removing the penis (penectomy).![]()

![]() Cystourethrectomy: Removal of the bladder, urethra, and nearby lymph nodes. This is typically done for more advanced cancers.
Cystourethrectomy: Removal of the bladder, urethra, and nearby lymph nodes. This is typically done for more advanced cancers.![]()

![]() Lymph node dissection: Removal of lymph nodes in the groin area to check for cancer spread.
Lymph node dissection: Removal of lymph nodes in the groin area to check for cancer spread.
![]() Radiation therapy: Using high-energy rays to kill cancer cells. It can be used alone or in combination with surgery or chemotherapy.
Radiation therapy: Using high-energy rays to kill cancer cells. It can be used alone or in combination with surgery or chemotherapy.
![]() Chemotherapy: Using drugs to kill cancer cells throughout the body. It may be used before or after surgery, or as the primary treatment for advanced cancer.
Chemotherapy: Using drugs to kill cancer cells throughout the body. It may be used before or after surgery, or as the primary treatment for advanced cancer.
![]() Immunotherapy: Using medications to help the body's immune system attack cancer cells.
Immunotherapy: Using medications to help the body's immune system attack cancer cells.
![]() Combination therapy: Using a combination of these treatments.
Combination therapy: Using a combination of these treatments.
Prognosis:
The prognosis (outlook) for urethral cancer varies depending on the stage of the cancer at diagnosis, the type of cancer, and the patient's overall health. Early detection and treatment are crucial for improving the chances of successful treatment and long-term survival.
Important Considerations:
![]() See a doctor: If you experience any symptoms that could be related to urethral cancer, it's essential to see a doctor promptly for evaluation.
See a doctor: If you experience any symptoms that could be related to urethral cancer, it's essential to see a doctor promptly for evaluation.
![]() Specialist: Treatment for urethral cancer is complex and should be managed by a team of specialists, including urologists, oncologists (cancer specialists), and radiation oncologists.
Specialist: Treatment for urethral cancer is complex and should be managed by a team of specialists, including urologists, oncologists (cancer specialists), and radiation oncologists.
![]() Follow-up care: Regular follow-up appointments are important after treatment to monitor for recurrence (cancer coming back).
Follow-up care: Regular follow-up appointments are important after treatment to monitor for recurrence (cancer coming back).
Disclaimer: This information is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.