Varicose Veins (Vascular Disease)
Published: 18 Jun 2025
ICD9: 454.8 ICD10: I83.899 ICD11: BD75.Z
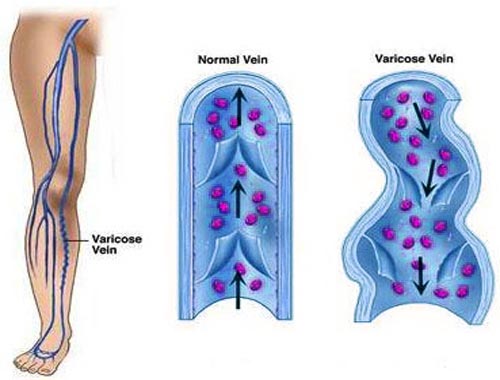
Varicose veins are enlarged, twisted veins that are visible just under the skin's surface.
They typically occur in the legs and ankles. While they can be unsightly and sometimes uncomfortable, they are usually not a serious medical problem for most people. However, in some cases, they can lead to complications. They fall under the broader category of vascular diseases.
Here's a breakdown of what you need to know about varicose veins as a type of vascular disease:
What are Varicose Veins?
![]() Description: Swollen, twisted veins, often appearing bluish or purplish. They are most common in the legs and ankles.
Description: Swollen, twisted veins, often appearing bluish or purplish. They are most common in the legs and ankles.
![]() Cause: The valves within veins that keep blood flowing toward the heart become weak or damaged. This allows blood to pool in the veins, causing them to enlarge and become varicose.
Cause: The valves within veins that keep blood flowing toward the heart become weak or damaged. This allows blood to pool in the veins, causing them to enlarge and become varicose.
![]() Appearance: Can look like bulging, rope-like structures beneath the skin. Smaller, thinner versions are called spider veins.
Appearance: Can look like bulging, rope-like structures beneath the skin. Smaller, thinner versions are called spider veins.
Why Do They Happen? (Causes and Risk Factors)
![]() Weak or damaged valves: The primary cause is malfunctioning valves in the veins.
Weak or damaged valves: The primary cause is malfunctioning valves in the veins.
![]() Age: Veins lose elasticity and valves weaken with age.
Age: Veins lose elasticity and valves weaken with age.
![]() Sex: Women are more likely to develop varicose veins, potentially due to hormonal changes (pregnancy, menstruation, menopause).
Sex: Women are more likely to develop varicose veins, potentially due to hormonal changes (pregnancy, menstruation, menopause).
![]() Pregnancy: Increased blood volume and hormonal changes during pregnancy can strain veins. The growing uterus also puts pressure on veins in the pelvis.
Pregnancy: Increased blood volume and hormonal changes during pregnancy can strain veins. The growing uterus also puts pressure on veins in the pelvis.
![]() Genetics: A family history of varicose veins increases your risk.
Genetics: A family history of varicose veins increases your risk.
![]() Obesity: Excess weight puts added pressure on veins, especially in the legs.
Obesity: Excess weight puts added pressure on veins, especially in the legs.
![]() Prolonged Standing or Sitting: Being in the same position for long periods can force veins to work harder to pump blood back to the heart.
Prolonged Standing or Sitting: Being in the same position for long periods can force veins to work harder to pump blood back to the heart.
![]() Other Factors: Prior leg injuries, blood clots, and tight clothing can also contribute.
Other Factors: Prior leg injuries, blood clots, and tight clothing can also contribute.
Symptoms
Not everyone with varicose veins experiences symptoms. When they do occur, they can include:
![]() Visible Bulging Veins: The most obvious symptom.
Visible Bulging Veins: The most obvious symptom.
![]() Aching or throbbing pain: Often described as a heavy or achy feeling in the legs.
Aching or throbbing pain: Often described as a heavy or achy feeling in the legs.
![]() Swelling: In the ankles and feet.
Swelling: In the ankles and feet.
![]() Burning, throbbing, muscle cramping and swelling in your lower legs
Burning, throbbing, muscle cramping and swelling in your lower legs
![]() Itching: Around the affected veins.
Itching: Around the affected veins.
![]() Skin discoloration: Particularly near the ankles and feet.
Skin discoloration: Particularly near the ankles and feet.
![]() Restless legs: A feeling of needing to move your legs, especially at night.
Restless legs: A feeling of needing to move your legs, especially at night.
![]() Leg heaviness or fatigue
Leg heaviness or fatigue
![]() In severe cases: Skin ulcers (sores), blood clots (thrombophlebitis), or bleeding.
In severe cases: Skin ulcers (sores), blood clots (thrombophlebitis), or bleeding.
Diagnosis
![]() Physical Exam: A doctor can usually diagnose varicose veins by visual examination.
Physical Exam: A doctor can usually diagnose varicose veins by visual examination.
![]() Duplex Ultrasound: A non-invasive test that uses sound waves to create images of the veins and check blood flow. It helps to determine the extent of the problem and rule out other conditions.
Duplex Ultrasound: A non-invasive test that uses sound waves to create images of the veins and check blood flow. It helps to determine the extent of the problem and rule out other conditions.
Treatment
Treatment options depend on the severity of the varicose veins, symptoms, and overall health.
![]() Self-Care Measures:
Self-Care Measures:![]()

![]() Compression Stockings: These help to support veins and improve blood flow.
Compression Stockings: These help to support veins and improve blood flow.![]()

![]() Elevation: Elevating the legs helps to reduce swelling and discomfort.
Elevation: Elevating the legs helps to reduce swelling and discomfort.![]()

![]() Exercise: Regular exercise improves circulation.
Exercise: Regular exercise improves circulation.![]()

![]() Weight Management: Losing weight can reduce pressure on veins.
Weight Management: Losing weight can reduce pressure on veins.![]()

![]() Avoid prolonged standing or sitting: Take breaks to move around.
Avoid prolonged standing or sitting: Take breaks to move around.
![]() Medical Procedures: When self-care isn't enough, more invasive treatments may be considered.
Medical Procedures: When self-care isn't enough, more invasive treatments may be considered.![]()

![]() Sclerotherapy: Injecting a solution into the vein to close it off.
Sclerotherapy: Injecting a solution into the vein to close it off.![]()

![]() Endovenous Laser Ablation (EVLA): Using laser energy to heat and close the vein.
Endovenous Laser Ablation (EVLA): Using laser energy to heat and close the vein.![]()

![]() Radiofrequency Ablation: Similar to EVLA, but uses radiofrequency energy.
Radiofrequency Ablation: Similar to EVLA, but uses radiofrequency energy.![]()

![]() Ambulatory Phlebectomy: Removing small varicose veins through tiny incisions.
Ambulatory Phlebectomy: Removing small varicose veins through tiny incisions.![]()

![]() Vein Stripping and Ligation: A more invasive surgical procedure to remove or tie off large varicose veins. This is less common now due to the availability of less invasive options.
Vein Stripping and Ligation: A more invasive surgical procedure to remove or tie off large varicose veins. This is less common now due to the availability of less invasive options.
Complications
While generally not dangerous, varicose veins can sometimes lead to complications:
![]() Thrombophlebitis: Inflammation of the vein with a blood clot.
Thrombophlebitis: Inflammation of the vein with a blood clot.
![]() Venous Ulcers: Open sores on the skin, usually near the ankles, due to poor circulation.
Venous Ulcers: Open sores on the skin, usually near the ankles, due to poor circulation.
![]() Bleeding: Varicose veins near the surface can bleed if injured.
Bleeding: Varicose veins near the surface can bleed if injured.
![]() Chronic Venous Insufficiency: Long-term condition where the veins are unable to pump enough blood back to the heart, leading to swelling, skin changes, and ulcers.
Chronic Venous Insufficiency: Long-term condition where the veins are unable to pump enough blood back to the heart, leading to swelling, skin changes, and ulcers.
Prevention
You can't completely prevent varicose veins, especially if you have a genetic predisposition, but you can reduce your risk:
![]() Maintain a Healthy Weight:
Maintain a Healthy Weight:
![]() Exercise Regularly:
Exercise Regularly:
![]() Avoid Prolonged Standing or Sitting:
Avoid Prolonged Standing or Sitting:
![]() Wear Compression Stockings: Especially if you're at high risk.
Wear Compression Stockings: Especially if you're at high risk.
![]() Avoid Tight Clothing:
Avoid Tight Clothing:
![]() Elevate Your Legs: When resting.
Elevate Your Legs: When resting.
Varicose Veins as a Vascular Disease:
Vascular diseases encompass any condition affecting the blood vessels (arteries and veins). Varicose veins are a specific type of vascular disease focusing on the veins. They are a manifestation of venous insufficiency, where the veins are not efficiently returning blood to the heart.
When to See a Doctor
It's important to see a doctor if:
![]() Your varicose veins are causing you pain or discomfort.
Your varicose veins are causing you pain or discomfort.
![]() You develop skin changes around the affected veins.
You develop skin changes around the affected veins.
![]() You notice signs of infection (redness, swelling, warmth).
You notice signs of infection (redness, swelling, warmth).
![]() You develop a sore or ulcer on your leg.
You develop a sore or ulcer on your leg.
![]() You have concerns about the appearance of your varicose veins.
You have concerns about the appearance of your varicose veins.
In summary, varicose veins are a common condition involving enlarged, twisted veins, usually in the legs. They are a form of vascular disease. They are often not serious, but can cause discomfort and, in some cases, lead to complications. Treatment options range from self-care measures to medical procedures. If you have concerns about varicose veins, consult a doctor.