Vasculitis, Angiitis, Arteritis
Published: 18 Jun 2025
ICD9: 447.6 ICD10: I77.6 ICD11: 4A44
Vasculitis, angiitis, and arteritis are all terms that refer to the same thing: inflammation of blood vessels.
They are essentially synonyms. The term used often depends on the specific type of blood vessel affected, the size of the vessels involved, and the underlying cause (if known).
Here's a breakdown:
![]() Vasculitis is the most general term, meaning inflammation of blood vessels.
Vasculitis is the most general term, meaning inflammation of blood vessels.
![]() Angiitis is another general term for inflammation of blood vessels. It is sometimes used interchangeably with vasculitis.
Angiitis is another general term for inflammation of blood vessels. It is sometimes used interchangeably with vasculitis.
![]() Arteritis specifically refers to inflammation of arteries (a type of blood vessel).
Arteritis specifically refers to inflammation of arteries (a type of blood vessel).
In essence, all three terms describe a condition where the walls of blood vessels become inflamed.
What happens in vasculitis (angiitis, arteritis)?
When blood vessels become inflamed, several things can happen:
![]() Narrowing of the Blood Vessels: The inflammation can cause the vessel walls to thicken, narrowing the space inside and reducing blood flow.
Narrowing of the Blood Vessels: The inflammation can cause the vessel walls to thicken, narrowing the space inside and reducing blood flow.
![]() Weakening of the Blood Vessels: The inflammation can weaken the vessel walls, leading to aneurysms (bulges) or even ruptures.
Weakening of the Blood Vessels: The inflammation can weaken the vessel walls, leading to aneurysms (bulges) or even ruptures.
![]() Blood Clots: Inflammation can promote the formation of blood clots within the vessels, further obstructing blood flow.
Blood Clots: Inflammation can promote the formation of blood clots within the vessels, further obstructing blood flow.
![]() Damage to Organs: Reduced blood flow due to narrowed or blocked vessels can damage the organs and tissues supplied by those vessels.
Damage to Organs: Reduced blood flow due to narrowed or blocked vessels can damage the organs and tissues supplied by those vessels.
Causes:
Vasculitis can be caused by a variety of factors, including:
![]() Autoimmune Diseases: Many types of vasculitis are autoimmune disorders, where the body's immune system mistakenly attacks its own blood vessels. Examples include rheumatoid arthritis, lupus, and scleroderma.
Autoimmune Diseases: Many types of vasculitis are autoimmune disorders, where the body's immune system mistakenly attacks its own blood vessels. Examples include rheumatoid arthritis, lupus, and scleroderma.
![]() Infections: Some infections, such as hepatitis B and C, can trigger vasculitis.
Infections: Some infections, such as hepatitis B and C, can trigger vasculitis.
![]() Medications: Certain medications can cause vasculitis as a side effect.
Medications: Certain medications can cause vasculitis as a side effect.
![]() Genetic Factors: In some cases, there may be a genetic predisposition to developing vasculitis.
Genetic Factors: In some cases, there may be a genetic predisposition to developing vasculitis.
![]() Idiopathic: In many cases, the cause of vasculitis is unknown (idiopathic).
Idiopathic: In many cases, the cause of vasculitis is unknown (idiopathic).
Symptoms:
Symptoms of vasculitis vary greatly depending on the type of blood vessels involved, the organs affected, and the severity of the inflammation. Common symptoms can include:
![]() Fever
Fever
![]() Fatigue
Fatigue
![]() Weight loss
Weight loss
![]() Muscle aches and pains
Muscle aches and pains
![]() Joint pain
Joint pain
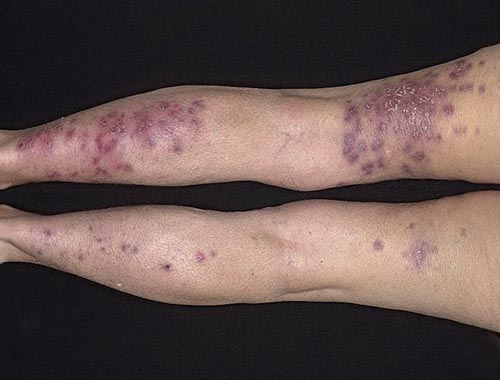
![]() Skin rashes
Skin rashes
![]() Nerve problems (numbness, tingling, weakness)
Nerve problems (numbness, tingling, weakness)
![]() Organ damage (e.g., kidney problems, lung problems)
Organ damage (e.g., kidney problems, lung problems)
![]() Headaches
Headaches
![]() Visual disturbances
Visual disturbances
Diagnosis:
Diagnosing vasculitis can be challenging because the symptoms are often nonspecific and can mimic other conditions. Diagnosis typically involves:
![]() Medical History and Physical Exam: The doctor will ask about your symptoms and medical history and perform a physical exam.
Medical History and Physical Exam: The doctor will ask about your symptoms and medical history and perform a physical exam.
![]() Blood Tests: Blood tests can help detect inflammation, identify autoimmune antibodies, and assess organ function.
Blood Tests: Blood tests can help detect inflammation, identify autoimmune antibodies, and assess organ function.
![]() Imaging Tests: Imaging tests such as X-rays, CT scans, MRI scans, and angiograms can help visualize the blood vessels and identify any abnormalities.
Imaging Tests: Imaging tests such as X-rays, CT scans, MRI scans, and angiograms can help visualize the blood vessels and identify any abnormalities.
![]() Biopsy: A biopsy of an affected blood vessel or organ can confirm the diagnosis of vasculitis.
Biopsy: A biopsy of an affected blood vessel or organ can confirm the diagnosis of vasculitis.
Treatment:
Treatment for vasculitis depends on the type of vasculitis, the severity of the condition, and the organs involved. Common treatments include:
![]() Corticosteroids: These medications help reduce inflammation.
Corticosteroids: These medications help reduce inflammation.
![]() Immunosuppressants: These medications suppress the immune system, which can help control autoimmune vasculitis.
Immunosuppressants: These medications suppress the immune system, which can help control autoimmune vasculitis.
![]() Other Medications: Other medications may be used to treat specific symptoms or complications of vasculitis.
Other Medications: Other medications may be used to treat specific symptoms or complications of vasculitis.
![]() Surgery: In some cases, surgery may be necessary to repair damaged blood vessels.
Surgery: In some cases, surgery may be necessary to repair damaged blood vessels.
Important Considerations:
![]() Vasculitis is a serious condition that can lead to significant health problems if left untreated.
Vasculitis is a serious condition that can lead to significant health problems if left untreated.
![]() Early diagnosis and treatment are essential to prevent organ damage and improve outcomes.
Early diagnosis and treatment are essential to prevent organ damage and improve outcomes.
![]() Treatment often requires long-term management and monitoring.
Treatment often requires long-term management and monitoring.
If you suspect you have vasculitis, it is important to see a doctor for diagnosis and treatment. A rheumatologist or vascular specialist are often involved in the diagnosis and management of vasculitis.